So, What Is a Low-FODMAP Diet?
Irritable bowel syndrome (IBS) may be a real pain in the rear. The chronic disease, which affects between 25 and 45 million individuals in the United States, is basically a collection of symptoms that cause havoc with your digestive system. Consider the following symptoms: discomfort, bloating, diarrhea, and/or constipation, to mention a few. As for therapy, the International Foundation for Functional Gastrointestinal Disorders states that although there are a variety of medicines available to help relieve IBS symptoms, lifestyle modifications such as changing your diet (wink, wink, nudge, nudge) are usually used as the first line of defense. And, as you’ve probably realized by now, this may include adhering to a low-FODMAP diet in order to achieve success. A low-FODMAP diet, however, is not as straightforward as it seems. And how does it function? Listed below, experts explain all you need to know about this gut-focused eating plan, including how it works and who should adhere to its recommendations.
I’ll say it right now: irritable bowel syndrome is a pain. The chronic condition affects between 25 and 45 million Americans and causes digestive issues. Consider: bloating, diarrhea, and/or constipation. The International Foundation for Functional Gastrointestinal Disorders says that while medications can help treat IBS, lifestyle changes like reevaluating your diet are usually the first line of treatment. And, as you’ve probably guessed, a low-FODMAP diet may be involved.
So, what is a low-FODMAP diet? What does it do? Here, experts explain how this gut-friendly diet works and who should use it.
What Are FODMAPs?
FODMAPs are a group of fermentable carbohydrates (starches, sugars, fiber) that can cause IBS-like symptoms like gas, bloating, diarrhea, constipation, and pain, according to Katie Thomson, M.S., R.D., co-founder and CEO of Square Baby, a nutritious baby food company. FODMAPS are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols that draw excess water into the small intestine and then move into the large intestine, where they’re fermented by bacteria that cause IBS-like symptoms (i.e. bloating, gas), says Thomson, who has IBS. For more information, visit CulinaHealth.com/water-and-gas-in-gut-contribute-to-altered-GI-motility. Only FODMAP-sensitive people (which, BTW, is not everyone with IBS). People who aren’t sensitive to FODMAPs “metabolize FODMAPs more efficiently,” so they don’t get the fluid retention.
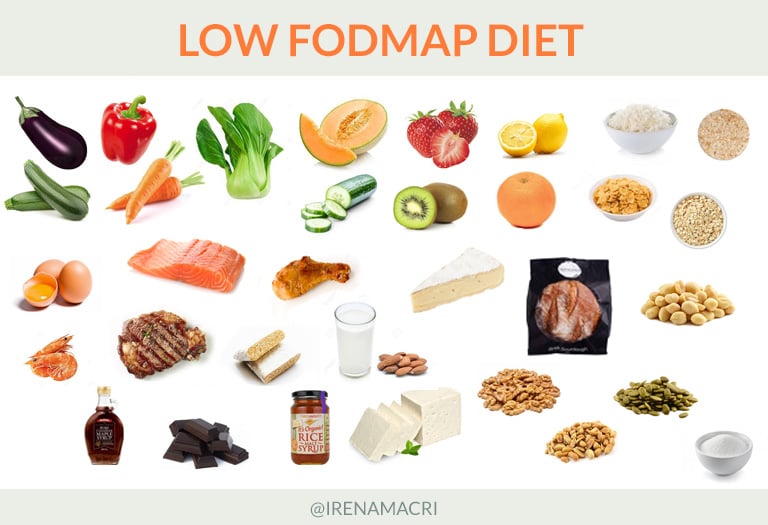
FODMAPS include gluten-containing grains (wheat, barley, rye), dairy products (especially milk and yogurt), as well as certain fruits and vegetables (i.e. apples, asparagus). Also, high-FODMAP suspects? Garlic and sugar alcohols (i.e. xylitol, sorbitol). Typical foods in each category, according to Thomson:
- Wheat, rye, and barley; beans and soy; almonds and cashews; dates and ripe bananas; Brussels sprouts, onions, and garlic.
- Lactose-containing foods like milk, yogurt, ice cream, and soft cheese.
- Apples, cherries, pear, figs, mango, asparagus, sugar snap peas, honey, agave.
- Apples, avocados, cherries, blackberries, figs, peaches, and plums contain polyols, as do sugar-free desserts and gum.
Why Eat Low-FODMAP Foods?
A low-FODMAP diet is not another trendy, ephemeral eating plan that requires calorie counting, macro counting, or any math at all. Instead, restrict (and then reintroduce) foods known to cause IBS-like symptoms. And it works: According to a 2016 scientific review, up to 86 percent of IBS patients find relief from their symptoms after following the eating plan.
“The diet’s goal is to help identify personal GI triggers,” Samuels says. So, how? “By eliminating FODMAPs and then reintroducing them,” she explains. Translation: removing a lot of foods from your diet (FODMAPs are in many foods) and then slowly reintroducing them to see which ones your gut can handle.
The low-FODMAP diet also allows your GI tract to heal, says Samuels. Taking a break from FODMAPs can help reduce inflammation caused by impaired motility (i.e. constipation and diarrhea), she explains.
According to Thomson and Samuels, this process can be broken down into three steps:
Remove high-FODMAP foods from your diet for two to six weeks, or until symptoms subside.
Symptom improvement allows you to “systematically reintroduce one FODMAP food/category at a time while tracking and monitoring your symptoms,” says Samuels. Apples, for example, contain polyols and fructose, making them poor test foods. Cauliflower, on the other hand, is “ideal for testing that category,” says Samuels.
This isn’t a reason to start pounding TJ’s cauliflower gnocchi (although, yum). Samuels recommends eating a normal-sized portion of the food for one meal per day for one to three days to test it. “If no symptoms appear after the first test, we increase the challenge food portion,” she says. “If symptoms occur, you go back to eating low-FODMAP for three days until the symptoms disappear.” During this phase, you should stick to the low-FODMAP diet except for the one category you’re reintroducing. (A food journal can help you keep track of your symptoms.)
After the reintroduction period, you can reintroduce any FODMAP category that you tolerated, says Samuels. So, if you passed the cauliflower test, you can reintroduce polyols.
Because everyone reacts differently to FODMAPs, some people may need to avoid or reduce certain IBS-triggering foods, while others can resume them without symptoms. Creating a nutrient-dense, balanced diet that works for you is the goal, says Thomson. So, to sum up…
Who Should Eat Low-FODMAP?
Yes, a low-FODMAP diet can help reduce IBS symptoms, but there’s a catch. “A low-FODMAP diet is not for everyone,” says Thomson. “Unless you have IBS, most FODMAPs are prebiotics, which feed good gut bacteria and help maintain a healthy microbiome.” Many of the foods considered FODMAPs are high in nutrients and fiber (fruits, veggies, legumes), so cutting them out won’t help your IBS symptoms.
A low-FODMAP diet may also be unsuitable for someone with an eating disorder. “Years of restricting food intake-either food groups like carbohydrates, when you eat, or calories,” says Samuels. “Restraining certain foods on the low-FODMAP diet can often trigger eating disorder behaviors in people with a history of eating disorders or disordered eating.”
However, you should always consult a nutritionist or doctor to see if this diet is right for you.